Going Further with the Global Malnutrition Composite Score
Interview with Peggy O’Neill, Vice President of Nutrition and Wellness for Morrison Healthcare
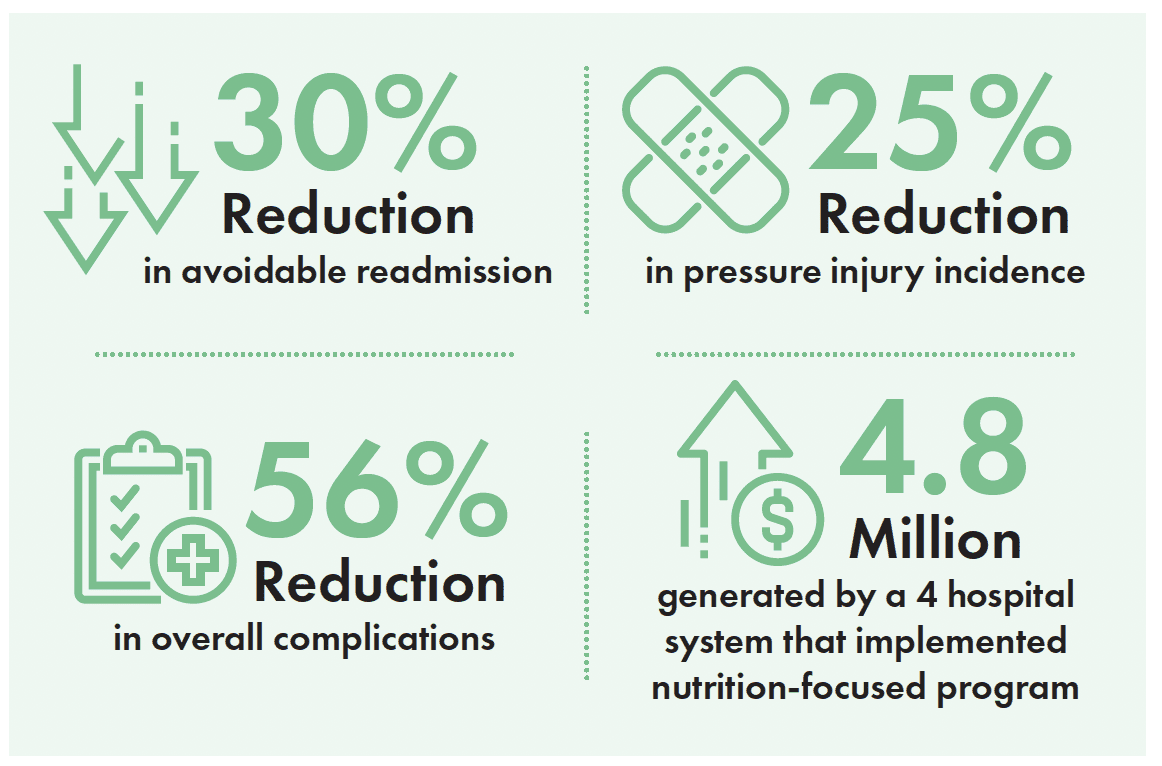
Morrison Healthcare’s MyMalnutrition program decreases length of stay and readmission rates for an at-risk patient population, and with the Global Malnutrition Composite Score, our clinical teams can go even further. In 2024, hospitals have the opportunity to report on GMCS as one of three voluntary self-selected eCQMs and are encouraged to screen all Medicare patients 65 and older upon admission. Hospitals who elect the GMCS metric will have an advanced focus on these patients, leading to increased reimbursement and improved patient outcomes, each of which result in healthcare cost avoidance. This is money that hospitals would not have if they were not targeting malnutrition.
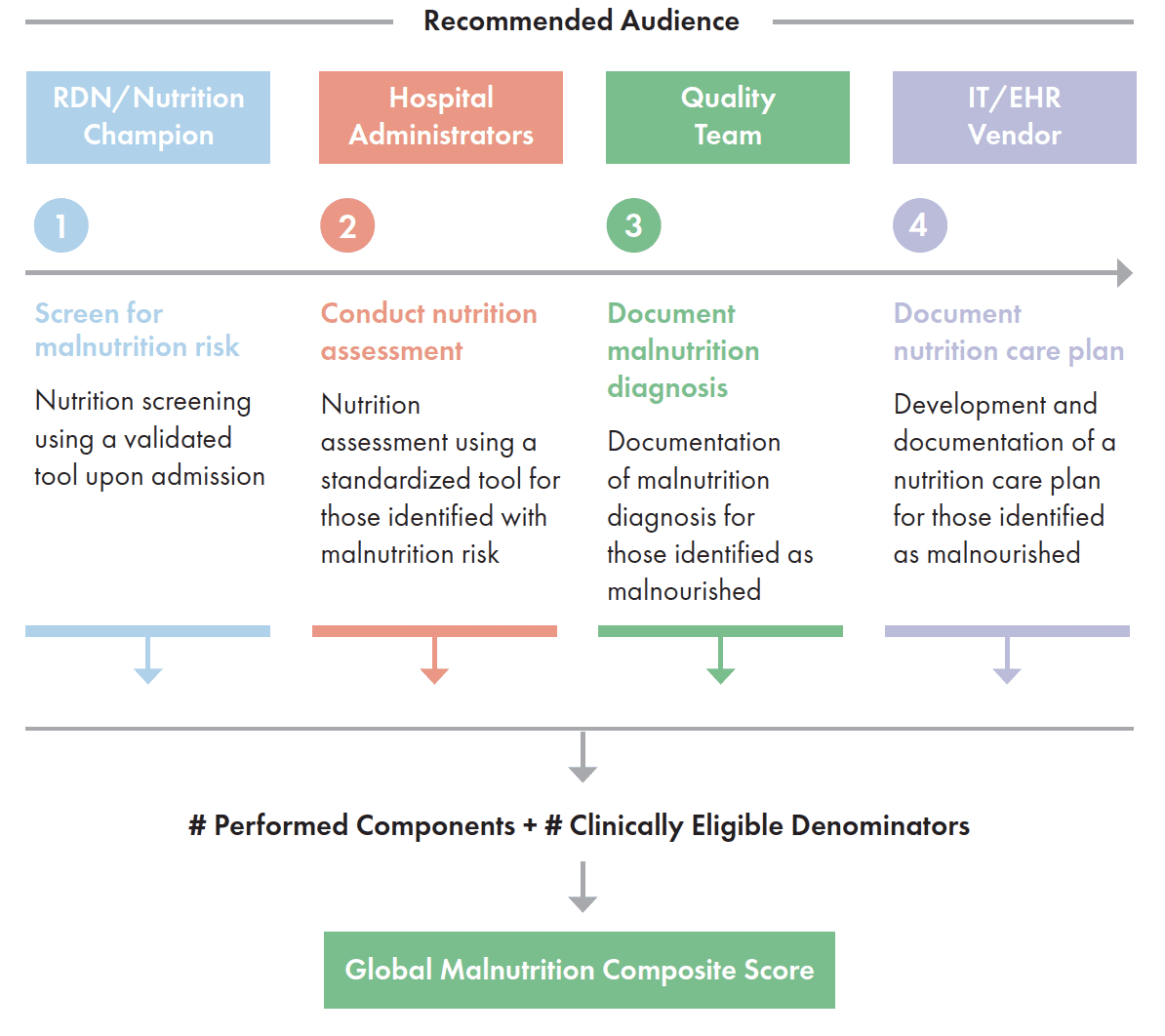
Early identification and treatment translates into cost savings for hospitals as we identify these patients, communicate the nutrition risk to physicians, add appropriate diagnostic codes, and bill accordingly. Why does early identification matter? Because roughly 30- 50% of hospitalized patients are malnourished upon admission— increasing the risk of falls, infections, and pressure injury—which in turn impact length of stay (LOS), hospital readmissions, and reimbursement rates. With the GMCS, we can expand our opportunities to identify malnourished patients (and those who are at-risk) through targeted screening, assessments, and documentation of the diagnosis. Our clinicians can then treat, develop targeted interventions, and help patients gain access to resources in their communities–while creating additional, significant, reimbursement opportunities. 10 to 15% of all diagnosed patients with malnutrition additional 5000 dollars in CMS reimbursement.
The Hospital IQR Program is a voluntary program that promotes the reporting of inpatient quality-of-care measures. Hospitals that meet all program requirements receive the full Medicare Annual Payment Update (APU), which is the yearly increase in Medicare payment rates for inpatient services. Hospitals that elect not to participate or that do not meet requirements do not receive the full APU.
Morrison Healthcare has continually developed industry-leading innovations and strategies to support their clinical dietitians in early identification of malnutrition, facilitating comprehensive nutrition care. Currently, our software helps dietitians and clinical nutrition managers track and analyze data, which is then used to identify, document, and treat more patients with malnutrition. With the GMCS, we can optimize missed opportunities, such as when a dietitian identifies malnutrition, but the patient wasn’t coded with malnutrition at discharge. And, for at-risk patients, these data insights are significant; they translate into support beyond the hospital walls. When asked, most of them reveal: “I might not eat”, or “I don’t have transportation or access to food.” Or, they say: “I do not have enough money for food.” We can go further with the data, both improving patient outcomes, prioritizing quality nutrition care– and preventing unnecessary readmission.
Hospital leadership will be selecting their voluntary clinical metrics during the coming months. Morrison Healthcare can support our clients to:
Hospitals that elect to report on the measure to CMS can leverage existing MQii resources to support them on their quality improvement journey.
As a leader with more than 700 hospitals and healthcare systems, Morrison Healthcare manages over 3000 Registered Dietitians focused on providing safe patient care and quality nutrition services that can help each hospital achieve lower readmissions, decrease length of stays, and reduced hospital acquired conditions, while optimizing cost savings and reimbursement opportunities.