Advancing Health Equity with Morrison Healthcare’s Targeted Malnutrition Program
Interview with Peggy O’Neill, Vice President of Nutrition and Wellness for Morrison Healthcare
Malnutrition touches all communities and is often under-identified in the hospital setting, which has implications for mortality, morbidity, functional decline, and increased hospital stays. Morrison Healthcare’s Malnutrition Program decreases length of stay and readmission rates for an at-risk patient population, and with the Global Malnutrition Composite Score, our clinical teams can go even further, advancing health equity with targeted interventions and a continuum of care.
Malnutrition is a highly preventable condition that does not strike communities evenly. The distribution of healthcare resources and social determinants of health underscores the prevalence of malnutrition in a community. Hospitals must be aware of their community’s risk factors and how unidentified malnutrition impacts healthcare outcomes.
- Up to 50% of patients at risk of becoming malnourished are affected by malnutrition
- 9% of hospitalized patients are diagnosed with malnutrition
- Up to 31% of malnourished patients and 38% of well-nourished patients experience a nutritional decline
Malnutrition represents a substantial burden to hospitals, requiring targeted initiatives to drive change within the hospital walls and beyond. Recent findings demonstrate a marked increase in hospital mortality readmission and length of stay due to malnutrition.
- 5x maximum likelihood of in-hospital death compared to the general patient population
- 56% higher likelihood of 30-day readmissions with septicemia as the leading diagnosis upon readmission
- 34% higher costs for a malnourished patient hospital stay compared to non-malnourished patient stays
Malnutrition prevention requires a holistic view of the challenge and relevant solutions that address the root causes of health inequity. The COVID-19 pandemic highlighted disparities already prevalent in our communities, demonstrating the need for health policy funding and interventions to address social determinants of health—and our targeted initiatives can guide policymakers in designing more permanent approaches. Morrison Healthcare has developed innovative and responsive malnutrition programs that drive results for patients, hospitals, and communities. Early identification of malnutrition improves the velocity at which clinicians can develop treatment plans to improve wellness.
 With an intentional malnutrition strategy, hospitals benefit from significant cost savings that result from improved patient outcomes.
With an intentional malnutrition strategy, hospitals benefit from significant cost savings that result from improved patient outcomes.
- 27% reduction in 30-day readmission rates for a multi-hospital Accountable Care Organization that optimized its malnutrition care.
- $4.8M in cost savings generated by a 4-hospital system that implemented a nutrition-focused quality improvement program.
- 24% relative reduction in readmission risk for malnourished patients with a nutrition care plan versus those patients without a care plan.
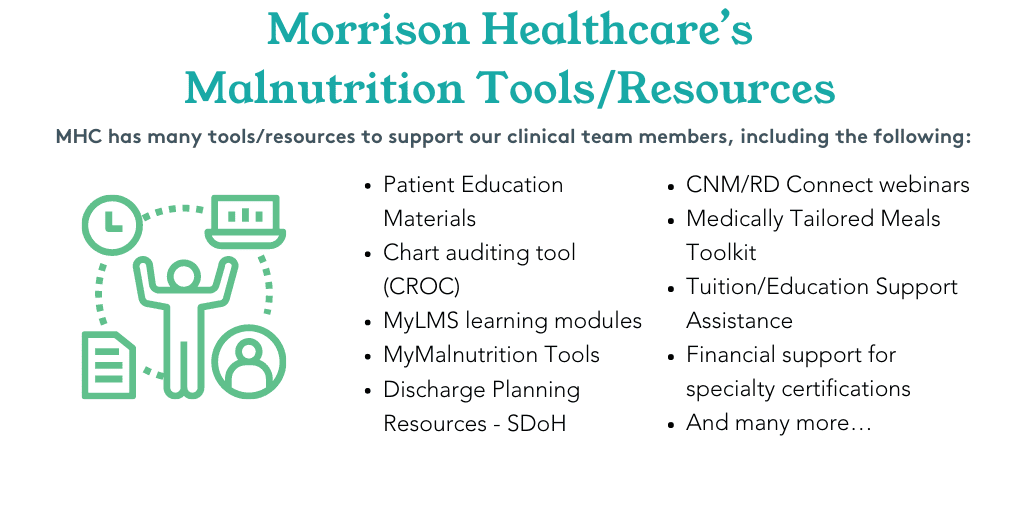
Moving forward, many hospitals are implementing Global Malnutrition Composite Score information (GMCS) into their data collection process and using that information to guide their improvement initiatives. In 2024, hospitals have the opportunity to report on GMCS as one of three voluntary self-selected eCQMs and are encouraged to screen all Medicare patients 65 and older upon admission. Many Morrison Healthcare clients plan to implement GMCS, which aligns with existing software, helping dietitians and clinical nutrition managers track and analyze data. Through this, we can better identify, document, and treat patients with malnutrition.
GMCS aligns with CMS priorities and meets additional health equity requirements, allowing hospitals to maximize reimbursements through enhanced clinical care, reduced length of stay, and improved patient experience. As part of a comprehensive population health strategy, GMCS can help healthcare leaders address health equity challenges through actionable data in your hospital.
—
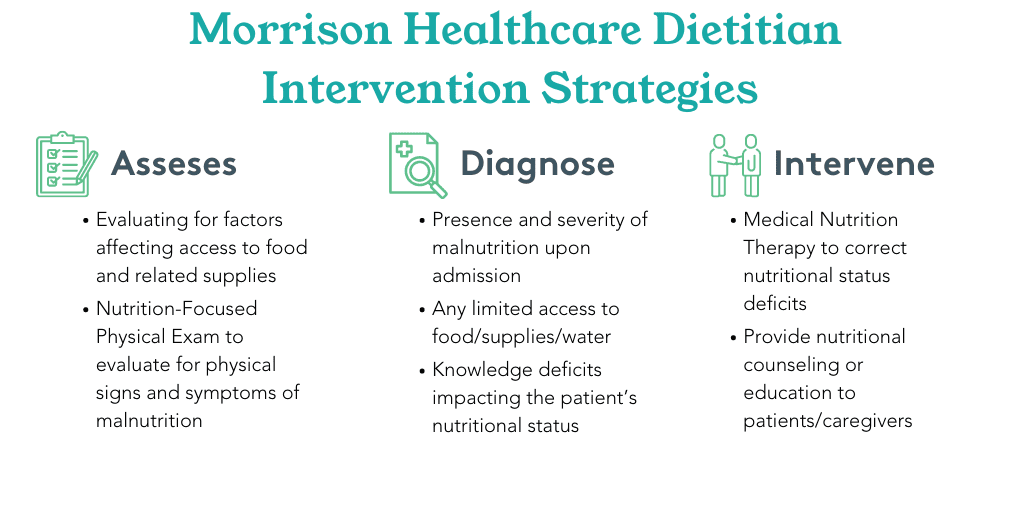
Implementing a Malnutrition Quality Improvement program involves getting the right data sets and developing dynamic strategies that address a facility’s unique needs. The steps include:
- Work with the Quality Improvement Department to assess the hospital’s malnutrition care processes and compare them to the standard nutrition care process workflow
- Identify and prioritize a malnutrition care process and documentation improvement
- Create and implement a plan with the care team to address prioritized areas for the malnutrition care process and documentation improvement