Health systems across the country are seeing improvement in patient outcomes and increases in revenues after implementing Morrison Healthcare’s Malnutrition Program.
In the past year alone, this tool has enabled partnering hospitals to capture $28 million in revenue based on accurate coding and subsequent billing. The program focuses on early identification, intervention, and appropriate documentation of malnutrition.
“If malnutrition is coded in a patient’s record properly, the hospital will be reimbursed at a higher level by the federal government for Medicare patients. Then those patients receive the care they need and can stay in the hospital for treatment longer without adding to the financial burden of the hospital,” explained Peggy O’Neill, Vice President of Nutrition and Wellness at Morrison Healthcare.
Consider the outcomes at a hospital system in the Northeast. The organization implemented the Malnutrition Program system-wide halfway through FY18. By FY19, they saw an increase of $12 million in revenue.
At that location, a Morrison Healthcare dietitian worked with a team of Registered Dietitian Nutritionists (RDNs), physicians, and coders and educated them on the accurate diagnosis and documentation of malnutrition.
“We wanted to make sure if we were going to pursue the malnutrition coding piece that we were doing it carefully, that we were billing for actual work and treatment completed the right way. The billing piece was very important for us, and we made sure we were clear from a compliance perspective,” said an executive from the health system.
Benefits of the Malnutrition Program
- Increased revenue. Our proprietary gap analysis methodology for malnutrition diagnosis and coding utilizes existing data and compares it against national benchmarks to project outcomes that are dependent on a multitude of hospital-level variables. Our corporate nutrition team can estimate the potential for increased reimbursement at your hospital based on information you provide, including:
- Total and Medicare annual discharges
- Percentage of patients coded with malnutrition upon discharge
- Case mix index
- Medicare standardized payment rate
A health system recognized that their malnourished patients had an above-average readmission rate at 40-68%. Within their hospitals, they identified that their malnourished patients had an average length of stay (ALOS) of 7.8 days, compared to an average length of stay of 4.3 days for non-malnourished patients. Based on this assessment, the health system implemented Morrison Healthcare’s Malnutrition Program.
This expansive health system has several locations, and the data is broken down by state. The initiative started in 2016 within the Virginia sites, and South Carolina was added in 2017.
Financial Outcomes:
Fiscal Year 2016 (VA only): $395,378
Fiscal Year 2017 (VA + SC): $735,336
Fiscal Year 2018 (VA+ SC): $1,333,073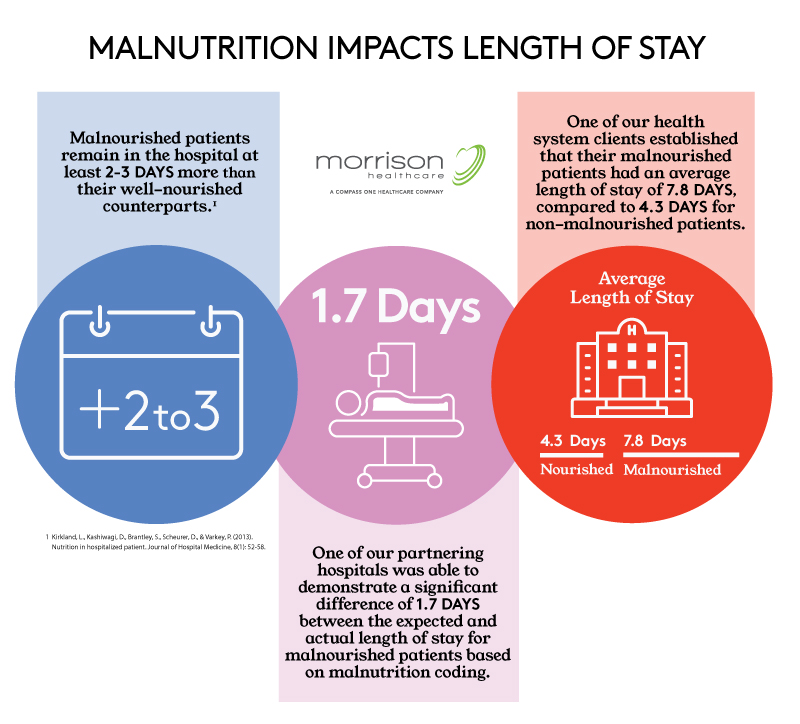
- Better patient outcomes. Patients with protein-calorie malnutrition remain in the hospital on average 5.8 days more than their well-nourished counterparts. Hospital costs associated with malnutrition are related to the average length of stay. Medicare establishes the expected average length of stay based on the final Medicare Severity-Diagnosis Related Group (MS-DRG), a system used to classify a patient’s hospital stay into various groups to facilitate payment of services.When malnutrition is identified, coded, and treated appropriately, the assigned MS-DRG may change, indicating a longer expected length of stay that more accurately reflects the resources needed to care for malnourished patients.
- Team-based care. The full application of the program allows clinicians to intervene early while working with the medical team and clinical documentation or coding specialists to ensure that the patient record accurately reflects the presence of malnutrition and the need to appropriately add malnutrition ICD-10 billing codes. An interdisciplinary team that includes representation from clinical nutrition, quality improvement, billing & accounting, coding/compliance specialist, and nursing work along with the medical director to establish the approved malnutrition criteria, ensure appropriate communication and training, and monitor the impact on patient outcomes and reimbursement. Most importantly, the patients receive high quality care and treatment because their malnutrition was identified early.
If you would like to learn more about the Malnutrition Program, please fill out the form below. The Morrison Healthcare corporate nutrition team could evaluate the potential of the impact of this program at your facility.




